The Great Realization
When I was young, I believed a doctor's word was gospel. However, as I delved into physiology and evidence-based practice, that reverence dissipated. While there are undoubtedly outstanding clinicians, therapists, and nurses, they're scarcer than I once thought. Over the years, my exposure to the darker side of healthcare has revealed a truly disconcerting reality.
Demystifying the Good Provider
It's a challenging realization because society often holds doctors in high esteem. Yet, this perception doesn't extend to the cook in a run-down restaurant. We almost accept dysentery as a calculated risk in such places. Conversely, we hold our healthcare providers in high regard, trusting them implicitly. This trust, perhaps, stems from a lack of understanding of science and evidence-based practice. Trust isn't always a conscious choice; for many, there's simply no other option. But what if this trust is misplaced? What if healthcare providers are no different from the cook at a dirty restaurant? And what’s worse, what if they spit in the food? That's the stark reality I witness regularly, and the more I learn, the more disheartening it becomes.
What Sets Me Apart
So, why am I positioned differently in this scenario? By now, you might be asking that question. If healthcare is flawed, what makes me one of the exceptions? For starters, I strive to keep my personal opinion out of the equation. I act as a conduit for reliable research. In my view, an exemplary healthcare provider channels and applies top-tier research to patients, producing the best outcomes. It's not about my opinion; it's about the consensus of intelligent minds, backed by numerous quality studies.
Secondly, I'm unapologetically devoted to medical study. Since obtaining my doctorate in physical therapy, my commitment to learning has only intensified. I've spent years refining anatomical drawings, depicting muscle origins, insertions, and relevant bone concavities with precision—a representation of what I consider perfect human anatomy (see picture below).
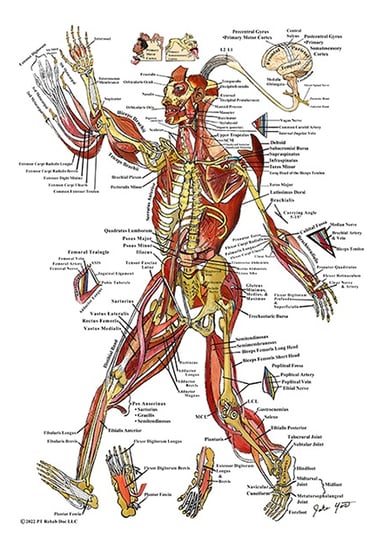
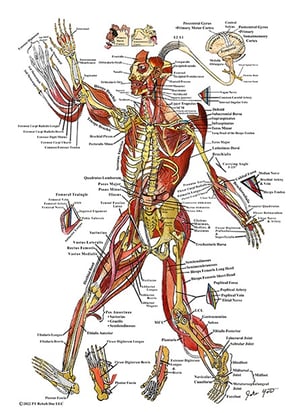
My home is adorned with such depictions, and my free time revolves around developing an online evidence-based practice platform aimed at addressing the issue of affordable healthcare (PTrehabdoc.com). In short, I'm likely one of the most passionate healthcare enthusiasts you'll encounter. Moreover, when faced with ethical dilemmas, I consistently choose the right path, even if it means jeopardizing my livelihood. My neck is on the line, and you're about to discover why. What I'm about to share is genuine but incredibly challenging to accept. I'm even contemplating recounting these stories under polygraph scrutiny with a body language expert. Otherwise, this information might be too hard to digest. So, without further delay, I present you the truth.
Accounts of the Truth
Unmasking Scabies in a Nursing Home: A Shocking Revelation
Let's begin with an unusual topic: scabies. I was at a nursing home with a locked memory care unit for patients with dementia. All 60 patients bore scars of scabies—tiny bugs that burrow under the skin and excrete feces, causing severe itching. The nursing staff discussed it in hushed tones. Occasionally, a nurse became infected, treated the scabies with permethrin and recovered, confirming Koch's postulates and solidifying the scabies diagnosis. However, patients only received Benadryl as treatment, but why?
In a nursing home, if 60 patients are diagnosed with scabies, fines are imposed, and star ratings drop. For over three years, the director of nursing, medical director, and administrator were complicit in purposefully misdiagnosing patients with contact dermatitis. Ethical care was sacrificed for corporate interests, with everyone, including the doctor, in on the conspiracy. Once, I asked the physician assistant why she participated. She grew quiet and uttered, "Oh, you know, the facility … ." She divulged nothing more.
A Tragic Cascade of Events
Another month passed, and the facility succumbed to a COVID outbreak. They put the COVID positive patients in the same room with COVID negative patients. Predictably, many patients died. Then, a fall-risk patient was left alone in the shower, slipped, hit his head on a pipe, began seizing, and died. They manipulated paperwork to suggest the seizure caused the fall. The corruption ran deep. I blew several whistles and even filed an anonymous complaint with the state, but inspectors didn't show up, and even if they did, change seemed unlikely. State inspectors lacked diligence, and hope dwindled. That's the harsh reality.
At some point, I knew the fight was over. I wanted to save these people, but as one person, I had to move on. I confronted my regional director that day, questioning her integrity. "You're either crooked, cold-hearted, or naive; I just don't know which," I told her. She clenched her fists and said, "I'm not naive." I responded, "Two out of three ain't bad," walked out, left, went home, took several showers, and found another job. That weekend, I vented my frustrations on the heavy bag, feeling like Sonny Listen's illegitimate offspring. It felt liberating.
You might think this was an isolated case, but it merely sets the tone of a pervasive pattern. Allow me to share another.
The Ignorance is Bliss Scenario: A Fart in the Shoulder
Let's transition from scabies to a peculiar incident: a "fart in the shoulder." While not as malevolent, it falls into the category of "ignorance is bliss." Nevertheless, it vividly illustrates the day-to-day challenges faced by conscientious clinicians—a testament to the pain of intellectual frustration.
The narrative unfolds with a patient I had been treating for weakness due to C. difficile infection—a severe condition causing excessive bowel movements. As you might have guessed, this patient was very weak in the legs so leg strengthening was typically our main focus. But one day, she confided that she could no longer lift her arm. She believed her shoulder was injured by the occupational therapist (OT) during their last treatment session.
As with any examination, I employed a systematic approach to avoid overlooking critical factors. I screened for general and joint-specific red flags, checked for edema or bruising, and scrutinized the cervical spine. Then, I assessed active thumbs-down scaption elevation, providing a Neer's test for impingement and a bird’s-eye view of the supraspinatus. This was followed by passive motion and additional special tests. The level of detail here is only a glimpse; it goes into extensive depth. The bear hug test alone, for instance, could warrant a book, considering its role in spotting tears in the subscapularis that may elude MRI and belly press tests. I've championed this stance since PT school, facing skepticism until recent research validated it nearly a decade later, but I digress. In short, this woman had signs of severe tears in her supraspinatus and infraspinatus.
Later, back at the gym office area, I delicately articulated my findings to the occupational therapist (OT). She fit the description of what I humorously term a "chairipist"—a therapist who rarely stands, spending her entire day seated, and at most, providing verbal instructions to patients. While I believe that the best approach is typically not the laziest one, this has become a somewhat common practice nowadays.
In the room, the OT was accompanied by an OT student. I took my time to compassionately explain the examination and results to the OT. To my surprise, she looked at me in front of her student and casually suggested, "Oh, it's probably gas. Yeah, seriously. I've seen doctors say it before. Gas from the stomach gets trapped in the shoulder. It's very painful." I paused for a moment, feeling a bit like I'd been hit with a BB gun. I was stunned by how this individual genuinely believed the issue was a fart in the shoulder. The mere existence of such a notion was disheartening.
I glanced over at the OT student, hoping to find a shared sense of disbelief, but the student sat there with a bubbly expression and gleaming brown eyes, fully endorsing the OT's conclusion. I resisted the urge to quip, "Excuse me for a moment; my shoulder needs to use the restroom. I'm sure you understand." However, it seemed futile. This OT and her student just misdiagnosed a serious injury to a woman's rotator cuff, and yet, they remained blissfully ignorant with metaphorical farts brewing in their shoulders. It was the epitome of the Dunning-Kruger effect—the psychological phenomenon where one is too unintelligent to recognize their lack of intelligence, especially dangerous when coupled with ego and authority.
A Silent Battle: The Unseen Struggles of a Diligent Therapist
This scenario exemplifies the plight of conscientious healthcare providers. The silent battles fought daily involve debunking misconceptions and navigating through an array of biases from misguided clinicians. While encountering the notion of a "fart in the shoulder" is a first for me, clinicians frequently dismiss patients' concerns, particularly when grappling with unfamiliar issues. The often-heard response is, "Are you sure it's not just in the patient's head?" Unfortunately, in this particular case, ignorance prevailed, and a woman with significant shoulder issues remained untreated. This is just one episode among many, underscoring the pervasive challenges faced by those committed to evidence-based practice.
Somehow, I could never reconcile with the accepted standard of wrongdoing, but many people find a way to accept it. A fairly bright physician once gave me some profound words. He emphasized that people, including doctors and nurses, are fallible—they make mistakes. While it made sense intellectually, I still harbored higher expectations for the medical profession. Then, there was this OT who once said to me, "Jake, misery is when expectations exceed reality, and happiness is when reality exceeds expectations." It resonated with me, and I desired contentment, but not at the cost of turning a blind eye to ethical concerns. While others found solace in career stability and acceptance in the standard of care, I yearned for positive outcomes driven by progressive scientific decision-making. In other words—I always wanted to do right by the patient.
Physicians in Focus: The Intelligence vs. Application Dilemma
Now, let's shift the spotlight to physicians because, in all fairness, it's not isolated to therapists. I have a notable example involving a highly esteemed surgeon I used to work with. His CV boasted a Mayo Clinic residency in sports medicine, a credential that often left people in awe. Unfortunately, what he possessed in prestige, he lacked in practical application. For a surgeon, he had no brains in his fingertips.
Challenging the Status Quo - A Critical Incident
One day, one of the surgeon’s patients came into the gym for an evaluation. As part of my routine examination, I checked for general red flags, starting with vitals. This woman presented with a resting blood pressure of 260/130 mmHg, indicative of a hypertensive emergency, accompanied by chest and jaw pain—classic signs of a heart attack. Without hesitation, I reached for the facility phone to call 911, but the surgeon intervened.
Ignoring Urgency: A Disturbing Encounter
The surgeon took the phone from me, looked me in the eye, and said, "I need you to do physical therapy on her arm. We do ortho here. We don’t do cardiac." I attempted to reason with him, but he seemed impervious to logic and accountability. Despite the potential consequences, I rushed back to the patient, informing her of the urgency and advising her to call 911 or have someone take her to the ER. She hesitated, having overheard the discussion, believing the doctor's assurance that she was fine. I didn't treat her, and she left.
Consequences Unveiled - A Patient's Perspective
A week later, I received a call on the facility phone from the patient. She apologized, admitting she had suffered a heart attack the next day, undergoing bypass surgery. She regretted not heeding my advice and acknowledged that I had tried to do the right thing. The situation escalated, and the doctor remained steadfast in his stance: "We don’t do cardiac here." Predictably, the doctor even went to great lengths to have me dismissed, but to no avail.
A Pervasive Issue - The Systemic Problem in Healthcare
Regrettably, such stories are far too common. While exceptional clinicians do exist, they are rare. Few are truly up-to-date with best practices, and those who are often find themselves ostracized. The prevailing ethos seems to be one of mediocrity, where like-minded individuals, perhaps lacking brilliance, form alliances.
Breaking Down the Illusion of Excellence in Medical Education
How does this happen in a field where admission to top schools is highly competitive? The answer lies in the fact that these coveted seats are often occupied by organized opportunists more interested in financial stability than the genuine pursuit of healthcare excellence. The selection process prioritizes test-taking prowess over genuine aptitude. And mediocrity wins in strength sense.
A Poignant Visual for Ethical Decision-Making
I'll leave you with one very important visual that I hope you never forget. At a long-term care facility, I encountered a man who hadn't walked for a decade. The man not only reeked of neglect, the flies buzzed around his bed as if he was already dead. A nurse popped her head in for 2 seconds and said to the patient, “You don’t wanna shower, right?” She left before he could even open his eyes. The man stared at me with flat affect as I pulled down his blanket. He reminded me of a Holocaust statue entitled The Unbowed Man, the way I could see the rivets in his sternum. At some point in my examination, I rolled the man onto his side and a thick layer of spider webs clung to his back, connecting his skin to the soiled bed sheets. It reminded me of times as a kid, peeling up rocks from the mud and looking under them. A broken spider staggered erratically across the bedding. It was a poignant reminder of two beings, both struggling to survive in their own ways.
Much of what I have written describes a grim scenario. My intention is not to indict the entire healthcare system or every practitioner. There are genuinely dedicated professionals striving for excellence. However, a cloak of silence often shrouds the injustices, allowing them to persist. My commitment to breaking this silence stems from a genuine desire to see positive change, to hold ourselves accountable to the principles of ethical care, and to foster a healthcare environment that truly prioritizes patient well-being. So I want you to remember that visual of the broken spider staggering across the man’s bed sheets. Just keep that in mind as you ponder the need for change.
Note: The information provided in this blog post is for educational purposes and should not replace professional medical advice. Always consult with a qualified healthcare professional for personalized guidance.
